IMMUNOLOGICAL AND RHEOLOGICAL DISORDERS IN PATIENTS WITH CHRONIC OBSTRUCTIVE PULMONARY DISEASE
DOBRYANSKIY D.V
COLLECTION OF SCIENTIFIC WORKS OF STAFF MEMBERS OF NMAPE, ED.17, KYIV, UKRAINE NATION’S HEALTH INSTITUTE LLC
SUMMARY
A comprehensive study of immunological and rheological changes provides the basis for a more detailed understanding of the pathogenesis of chronic obstructive pulmonary disease (COPD). The analysis of the immunogram of COPD patients showed significant heterogeneity and multiple vector of detected disorders, which was the basis for isolation of different types of immunopathological reactions. Among all patients with COPD, rheological blood flow abnormalities were observed in 74% of patients, with high blood viscosity syndrome found in 32% of them.
Keywords: immunology, rheology, immunodeficiency, complex, monoclonal antibodies, T-cell, lymphocytes, IgG, CD4.
INTRODUCTION
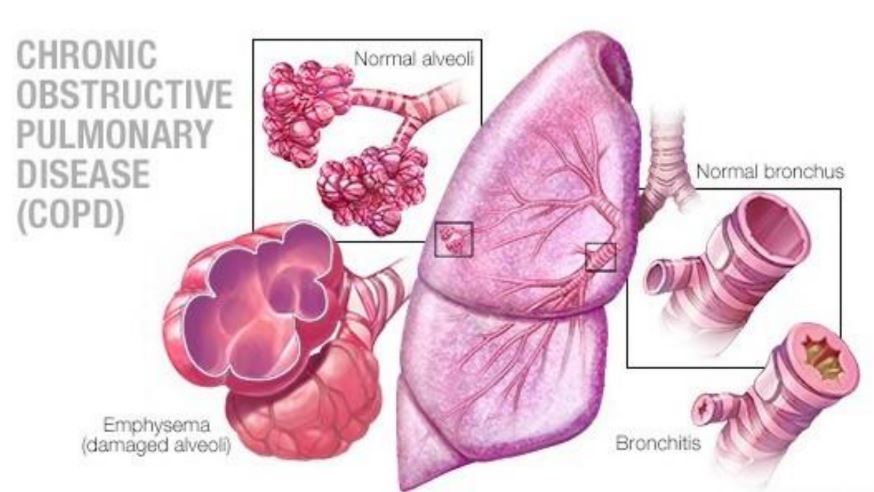
Chronic obstructive pulmonary disease is is one of the leading causes of morbidity and mortality worldwide. Recently, there has been a sharp increase in COPD incidence in Ukraine and an increase in disability and mortality rates [1,4].
As is known in the conditions of hypoxia, with excessive activation of free radical processes and lipid peroxidation, there is destabilization of the hemostasis system towards the increase of blood hemocoagulation potential [1, 3]. Due to the fact that the lungs are the main producer of thromboplastin, VII, VIII plasma factors, heparin and are involved in the transformation of megakaryocytes into platelets, hypercoagulative mechanisms in the progression of pathological processes in the bronchopulmonary system are rapidly progressing. Destabilization of platelet, vascular and coagulation units of hemostasis with impaired thus rheological characteristics of blood adversely affects perfusion and diffusion processes and pressure levels in the pulmonary artery. In turn, microcirculatory disorders and changes in oxygen homeostasis leads to destruction of the lipoprotein membrane complex, depression of the morpho-functional activity of cells, including immunocompetent cells. Under these conditions, the progressive suppression of cell-mediated and humoral immunity ends with the formation of immunodeficiency [5]. In case of increased secretion of leukocytes of proinflammatory mediators and interleukins, the process of activation of the coagulation unit of hemostasis and intensification of rheological disorders become progressive in nature and a “false circle” is formed.
A comprehensive study of changes in the state of hemostasis and the immune system and their comparative characteristics provide the basis for a more detailed understanding of the pathogenesis of this disease [2, 4].
The purpose of this work is to evaluate immunological and rheological disorders and their relationships in COPD patients.
MATERIALS AND METHODS OF RESEARCH
The condition of the hemostasis system was examined in 55 patients (15 women and 40 men) with COPD aged 38 to 67 years. An immunological study was performed in 96 COPD patients, 81 of them were men, 15 were women; age from 38 to 67 years. The control group consisted of 23 age-matched healthy volunteers. In all examined patients, the disease was in the acute phase. The study did not include patients with severe pulmonary insufficiency with FEV1 less than 30% of the appropriate value.
The diagnosis of COPD was established on the basis of clinical and radiological, laboratory and functional data according to the order of the Ministry of Health of Ukraine No. 499 of October 28, 2003.
In addition to generally clinical methods of examination, immunological reactivity and blood rheological properties were investigated.
Immunological examination of patients was carried out in the first 5 days after hospitalization and included: quantitative evaluation of T- and B-links of immunity by indirect immunofluorescence method using monoclonal antibodies against antigens of lymphocytes CD3, CD4, CD8, CD16, CD22 and endocrine cells of each phenotype (for 1 patient – 1000 cells); the study of the functional activity of T-lymphocytes by blast transformation reaction (RBTL) with PHA (Welcome Burroughs) by morphological method; study of the functional activity of B-lymphocytes by the production of serum IgG, IgA, IgM; study of a subpopulation of activated T-lymphocytes; determining the concentration of circulating immune complexes (CECs) of average size in serum using PEG-6000 on a Specol-21 microspectrophotometer (Germany) at a wavelength of 450 nm; study of the phagocytic activity of neutrophils by the degree of absorption of latex particles by calculating the phagocytic index (PI) of Hamburg and the phagocytic number (PN) of Wright [6].
The rheological properties of blood, which were determined on a rotary viscometer with a free-floating cylinder of the Zakharchenko system.
Rheological blood test includes evaluation of hematocrit (Ht), effective blood viscosity (ηα) at shear rates 1s-1 and 5s-1, erythrocyte viscosity (ηвн) at shear rates 1s-1 and 5s-1, as well as blood flow limits (τ0 ) and erythrocyte aggregation rate (КАер).
Statistical processing of the results obtained using the standard package “MS Excel”.
RESULTS AND DISCUSSION
Given current views on clinical and immunological studies, the definitions of the immunodeficiency state should take into account the peculiarities of the disease, the patient’s age and the time of year when the immunological study was conducted.
As evidenced by the analysis of the baseline data of immunological status in patients with COPD during the exacerbation, the most significant is the disturbance on the part of the cellular link, which vary depending on the individual features of the reactivity of the immune system. In this case, the average statistical subpopulations of T- lymphocytes, as a rule, approach the indicators of the control group. The most characteristic feature of the immunogram in all patients during COPD exacerbation is
the reduction of natural killer cells and the inhibition of the phagocytic activity of neutrophils, as well as the IgG, IgA and IgM hypoimmunoglobulinemia.
Established immunological disorders, as well as marked features of clinical manifestations can be regarded as a sign of immunopathological condition. During the analysis of the immunogram data of patients with COPD, significant heterogeneity and heterogeneity of the detected disorders were noted, which was the basis for the isolation of different types of immunopathological reactions, all examinations were divided into three subgroups: with hyperergic, hypoergic type and immunomodulitis (Table 1).
Table 1.
Average values (M ± m) of the immunogram
|
Data |
The control group (n-23) |
Hyperergic reaction (n-19) |
Hypoergic reaction (n-15) |
Some violations (n-62) |
|
Absolute lymphocyte count |
2,41± 0,23 |
3,19± 0,12* |
1,23± 0,07* |
2,13± 0,07 |
|
СD3+ |
1,59± 0,17 |
2,06± 0,10* |
0,66± 0,09* |
1,27± 0,06* |
|
СD4+ |
0,86± 0,04 |
1,39± 0,10* |
0,36± 0,04* |
0,8± 0,05* |
|
СD8+ |
0,52± 0,03 |
0,74± 0,02 |
0,3± 0,06* |
0,49± 0,02* |
|
Тх/Тс |
1,81± 0,19 |
2,25± 0,14* |
1.43±0,19 |
1,97±0,29* |
|
Таcт. |
0,59± 0,06 |
1,47± 0,14* |
0,43± 0,02* |
0,88± 0,05 |
|
СD22+ |
0,39± 0,04 |
1,16± 0,09* |
0,38±0,05 |
0,71±0,03* |
|
СD16+ |
0,46± 0,05 |
0,44± 0,02 |
0,23± 0,03* |
0,3± 0,02* |
|
LBTR |
1,68± 0,18 |
2,59± 0,10* |
0,91±0,11* |
1,67±0,06 |
|
mLBTR |
0,04± 0,003 |
0,09± 0,004* |
0,04±0,008 |
0,06±0,01* |
|
IgG |
13,8± 1,45 |
8,45± 0,17* |
8,66± 0,43* |
8,42± 0,3* |
|
IgA |
2,02± 0,24 |
1,27± 0,06* |
1,39±0,17 |
1,38±0,05* |
|
IgM |
0,76± 0,02 |
0,81± 0,04 |
0,85± 0,07 |
0,83± 0,03* |
|
PI |
69,8± 7,2 |
65,7± 1,87* |
66,2± 3,52* |
65,5± 0,79* |
|
CEC |
51,7± 3,17 |
61± 0,93* |
60,3± 0,8* |
61±0,58* |
Note: * The difference is likely compared to the control (p <0.05).
Hyperergic type of immunodeficiency was detected in 19 patients, it was characterized by an increase in the absolute number of lymphocytes, subpopulations of CD3+ -, CD4+ -, CD8+ -lymphocytes activated by T-lymphocytes, as well as their proliferative activity. Hyperactive reaction of the immune response in the case of prolonged persistence of high-level immune constants can lead to allergy and transform COPD into bronchial asthma.
Hypoergic type of immunodeficiency established in 15 patients, which indicates the depletion of the immune response, manifested by a decrease in both the humoral and cellular level of immunity mainly by reducing subpopulations CD3+-, CD4+-, CD8+-, CD16+-lymphocytes and IgG and IgA concentrations in the blood. Hypoergic type of immunodeficiency is a sign of decompensation of the immune response, which is an undoubted reason for carrying out the immune correction.
All other patients (62) experienced immune deficiency in some units. Thus, in 16 patients there was insufficiency of mainly helper function (CD4+ lymphocyte count) with low immunoregulatory index, in 12 patients insufficiency of suppressor function with high immunoregulatory index was insufficient, in 24 patients there was marked insufficiency of cell count and their proliferative activity). The results can be explained by the different direction of the immune response, depending on the compensatory capacity of the organism and the features of the etiopathogenesis factors and the degree of respiratory failure and the severity of the inflammatory reaction.
Among all COPD patients, hemorrhagic abnormalities were detected in 74% of patients, with 32% of those with high blood viscosity syndrome.
https://newsnetwork.mayoclinic.org/
As can be seen from the data presented in Table 1, the examined patients revealed significant abnormalities on the basis of the basic parameters of the hemorheogram, as evidenced by a significant increase in the level of hematocrit (Ht), effective blood viscosity and internal erythrocyte viscosity at a shear rate of 1s-1, as well as blood and the erythrocyte aggregation rate.
Table 2.
Average values (M ± m) of rheological characteristic
|
Data |
Control group (n – 23) |
Clinical group (n – 55) |
|
Ht, % |
47,62±0,56 |
49,80±0,46* |
|
ηα1s1, MPa·s |
9,60±0,17 |
11,78±0,42* |
|
ηα5s1, MPa·s |
4,17±0,06 |
4,64±0,17 |
|
ηвн1s1, MPa·s |
18,10±0,38 |
21,36±0,77* |
|
ηвн5s1, MPa·s |
6,60±0,12 |
7,16±0,33 |
|
τ0, MPa·s |
3,58±0,20 |
5,51±0,45* |
|
КАер, MPa·10-5 |
5,43±0,33 |
7,55±0,46* |
Note: * the likelihood of a difference from the control (p <0.05)
A statistically significant increase in hematocrit level has a negative effect on the kinetic activity of the blood, the Z-potential of erythrocytes and the morphology and functional activity of endothelial cells. The enhancement of the retention, aggregation capacity of the shaped elements and the induction of blood coagulation potential contribute to the growth of circulatory disorders at the level of the microcirculatory bed and the progression of endo- and intravascular pathomorphological changes. This is confirmed by a 16% increase in erythrocyte intrinsic viscosity at a shear rate of 1s¹, which corresponds to blood circulation in the postcapillaries. Compared with the healthy group, COPD patients showed a 24% increase in apparent blood viscosity. The increase in the aggregation capacity of erythrocytes by 30%, noted by us, contributes to the increase of pathological aggregation of the formed elements of blood.
The release of excess erythrocyte bioactive substances is one of the reasons for the formation of intravascular conglomerates of blood cells, the occurrence of occlusion of the microcirculatory bed and the violation of the perfusion and diffusion capacity at the level of the bronchial pulmonary apparatus.
Numerous studies point to the close interrelation of the immunity system and hemorheology, but the integral mechanisms of these linkages are still poorly understood. The influence of immunological factors on the processes of blood clotting, especially in a state of hyperreactivity, is clearly reflected in blood clotting and its strength characteristics. A correlation analysis was performed to evaluate the immunological and rheological relationship. According to the results of complex correlation analysis, without taking into account the stage of COPD and the severity of inflammatory changes and the type of immune response, the correlation was very weak, not exceeding 0.2. In a detailed analysis of the subdivision of patients into subgroups with regard to individual characteristics, the correlation between individual indicators of hemorrhage and immunogram exceeded 0.5, which is estimated as a correlation relationship of the average degree.
CONCLUSIONS
-
All COPD patients have multiple vector disorders of immunological parameters, but the most characteristic is the reduction of natural killer (NK) cells and inhibition of the phagocytic activity of neutrophils, as well as hypoimmunoglobulinemia IgG, IgA and IgM.
-
Violation of hemorheological characteristics of the blood was noted in 74% of the surveyed, with 32% of them showed a syndrome of high blood viscosity.
-
A large number of scientific studies can confirm the hypothesis of the relationship between immunity and hemorheology, but a detailed analysis did not find a strong correlation between these indicators.
REFERENCES
-
Feshchenko YI., Yashina LA., Polyanskaya AM., Mist A.N. Obstructive pulmonary disease. // Educational program for doctors. – Kiev, 2004. – 287 p.
-
Dudka PF, Ilnitsky RI, Dobryansky DV, Sokolova LI, Bychkova NG, Bryuzgina TS Contemporary views on the place of antigomotoxic agents in the treatment of chronic obstructive pulmonary diseases // Problems of military health care: a collection of scientific papers of the Ukrainian Military Medical Academy. Issue 15. – Kiev, 2006. – P. 155-160.
-
Dudka PF, Ilnitsky RI, Sokolova LI, Dobriansky DV, Valikhnovskaya. N.B. Hemomicrocirculatory disorders and their correction in patients with chronic obstructive pulmonary disease // Ukrainian Journal of Pulmonology. – 2007. – №1. – P. 17.
-
Chuchalin AG Chronic obstructive bronchitis (definition, etiology, pathogenesis, clinical picture, therapeutic program) // Ter. archive.- 1997.- № 3.- P. 5-9.
-
Jakobysiak M. Immunology (Translated from Polish by Prof. VV Chopyak. – Vinnitsa: New Book, 2004. – 672 p.).
-
Prederiy VG, Zemskov AM, Bychkova NG. Immune status, principles of its evaluation and correction of immunological disorders. K .: Health, 1995. – 211 p.
